Background:
One of the major long-term complications in aplastic anemia (AA) is the clonal evolution to secondary myeloid neoplasms (sMNs) such as acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) 1. Hematopoietic stem cell transplantation (HSCT) is largely considered a curative treatment option for AA and is effective at preventing the clonal evolution of sMNs 2. However, patients over 40 years old or those with poor donor options are contraindicated for HSCT due to elevated post-transplant mortality rates 3. When treated with non-transplant strategies, patients with AA have indeed a high risk for acquisition/expansion of somatic myeloid mutations, with some harbingers of future clonal progression to full-blown MDS or AML. Older age, presence of myeloid mutations other than BCOR/L and PIGA at onset, and lack of response to standard immunosuppressive treatment (IST) have been identified as factors predictive for subsequent sMN evolution 4,5,6. If an individual patient's risk of developing a sMN could be assessed through a predictive model that uses information collected at initial AA diagnosis, providers may consider HSCT for traditionally contraindicated patients. However, no such predictive model that could aid in risk assessment currently exists.
Methods:
In our study, we utilized a large, multi-institutional cohort of patients diagnosed with AA to generate a comprehensive dataset. This dataset contained 76 variables, encompassing relevant clinical and molecular annotations. On this dataset, we trained a machine learning (ML) model to predict patients who would evolve sMNs. Variables with the highest feature impact score (FIS) in predicting clonal evolution to sMN were then chosen to be included in the final ML model, and the algorithm's fitness was calculated using the Leave-One-Out cross-validation method. Variables missing in more than 30% of subjects were imputed using K-Nearest Neighbors (N=20).
Of our initial cohort of 455 patients, 213 patients were excluded from the study. 35 patients were excluded because they were treated with HSCT. 39 pediatric cases (defined as <18 years old at the time of diagnosis) were excluded from the study. 91 patients were removed for not receiving specific treatment (IST or HSCT). The remaining 77 patients were excluded due to having a sMN detected at the time of or prior to AA diagnosis, insufficient data, or detection of a germline mutation indicative of an inherited pathophysiology. Our final cohort included a total of 242 acquired AA patients from UT Southwestern Medical Center and Cleveland Clinic.
Results:
Among our final cohort of 242 patients, 119 (49.2%) were male. The cohort's mean and median ages at AA diagnosis were 53.1 years (SD = 18.9 years) and 58.1 years, respectively. The median follow-up time was 4.04 years. 80 (33.1%) of our patients had a clinically significant PNH clone (defined as >0.001%). 29 patients developed sMNs, with 24 developing MDS and 5 developing AML. Of patients who underwent clonal evolution to sMNs, the median age at the time of AA diagnosis and sMN diagnosis was 63.1 years and 67.2 years, respectively. The median time elapsed from initial AA diagnosis to sMN evolution was 3.78 years. The median time elapsed between initial AA diagnosis and earliest IST administration was 51 days. Chi-squared analysis showed that patients who received ATG treatment were more likely to develop sMNs, with 78.0% of all patients receiving ATG, while 96.6% of patients who developed sMNs had received ATG (p=0.00927).
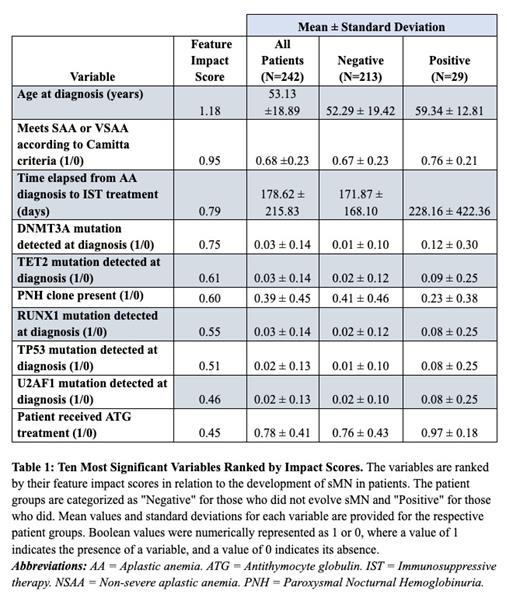
Our ML model achieved a sensitivity of 0.759, a specificity of 0.728, and an AUC of 0.78 using the ten variables with the highest feature impact score (FIS) to predict clonal evolution [Table 1]. All of the variables except for the presence of a PNH clone are positively correlated with sMN evolution. Nine of these variables are supported by existing literature 7,8. The feature with the third highest feature impact score, the time elapsed (days) between diagnosis and IST treatment, has not been established by previous studies and may be an important consideration in establishing optimal AA treatment guidelines.
Conclusion:
The strategic combination of this ML algorithm with clinical expertise has tremendous potential in improving health outcomes. Identification of patients at high risk for sMN and offering HSCT as a curative option upfront may lead to improved overall survival in AA patients.
Disclosures
Bat:Alexion pharma: Membership on an entity's Board of Directors or advisory committees. Maciejewski:Novartis: Honoraria, Speakers Bureau; Alexion: Membership on an entity's Board of Directors or advisory committees; Regeneron: Consultancy, Honoraria; Omeros: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal